ABSTRACT
INTRODUCTION: Late effects of radiation are generally irreversible and can have devastating effects on quality of life of people exposed either accidentally or during therapeutic radiation treatments. Although many etiologies have been suggested regarding these late toxicities, inflammatory parameters involved during the late phase are less known.
OBJECTIVE: The aim of this study was to analyze the response of the immune system in the inflammatory reactions in patients with late skin injuries after radiotherapy or interventional fluoroscopy procedures.
METHODS: The follow up of twenty five patients, out of 160 referred to Burn Hospital from 1997, that showed late cutaneous reactions graded according to the RTOG / EORTC system is reported here.The expression of adhesion molecules ICAM1 and β1-integrin on granulocytes and lymphocytes, as well as changes in subpopulations of T lymphocytes were evaluated by flow cytometry and the level of C-reactive protein, a well-studied inflammatory marker was quantified by an immunoturbidimetric assay.
RESULTS: The analysis of adhesion molecules expression revealed a higher expression of β1 Integrin on lymphocytes of Grade IV patients compared to non-exposed controls. It was also noted a decrease in its expression values in the follow up of patients with good response to therapeutic treatment. This was paralleled by a tendency to a decrease in the T(CD4+) / T(CD8+) ratio of G4 patients with bad evolution compared to G4 patients with good evolution.The level of C Reactive Protein (CRP) showed higher values in patients in acute phase and patients with late toxicity but in exacerbation crisis.
CONCLUSIONS: The parameters analyzed, which require confirmation in a larger study, in combination with other inflammatory indicators, could be used as potential follow-up markers of the chronic radio-induced inflammation process just as its response to therapeutic treatments.
Keywords:
Radiation. Inflammation. Immune system. Cell adhesion molecules.
RESUMO
INTRODUÇAO: Os efeitos tardios da radiaçao geralmente sao irreversíveis e podem ter efeitos devastadores sobre a qualidade de vida de pessoas expostas acidentalmente ou durante os tratamentos de radiaçao terapêutica. Apesar de diversas etiologias terem sido sugeridas em relaçao a essa toxicidade tardia, parâmetros inflamatórios envolvidos durante a fase tardia sao menos conhecidos.
OBJETIVO: O objetivo deste estudo foi analisar a resposta do sistema imunológico nas reaçoes inflamatórias em pacientes com lesoes de pele tardias após radioterapia ou procedimentos de fluoroscopia intervencionista.
MÉTODOS: O acompanhamento de 25 pacientes, dos 160 atendidos no Hospital de Queimados a partir de 1997, que demonstrou reaçoes cutâneas tardias classificadas de acordo como sistema de RTOG/EORTC é relatado aqui. A expressao de moléculas de adesao ICAM1e β1-integrina em granulócitos e linfócitos, bem como alteraçoes nas subpopulaçoes dos linfócitos T, foram avaliadas por citometria de fluxo e o nível de proteína C-reativa, um marcador inflamatório bem estudado, foi quantificado por um ensaio imunoturbidimétrico.
RESULTADOS: Aanálise da expressao de moléculas de adesao revelou maior expressao de integrina β1em linfócitos de pacientes Grau IV em comparaçao a controles nao-expostos. Observou-se, também, diminuiçao dos valores de sua expressao no acompanhamento de pacientes com boa resposta ao tratamento terapêutico. Isto foi acompanhado por uma tendência a diminuiçao na proporçao T (CD4 +)/ T(CD8+) de pacientes com má evoluçao do G4 em comparaçao aos doentes do G4 com boa evoluçao. O nível de proteína C reativa (PCR) apresentou valores mais elevados em pacientes em fase aguda e pacientes com toxicidade tardia, mas em crise exacerbaçao.
CONCLUSOES: Os parâmetros analisados, os quais requerem a confirmaçao de um estudo maior, em combinaçao com outros indicadores inflamatórios, podem ser utilizados como potenciais marcadores de seguimento do processo de inflamaçao crônica induzida por radiaçao, tal como a sua resposta aos tratamentos terapêuticos.
Palavras-chave:
Radiação. Inflamação. Sistema imunológico. Moléculas de adesão celular.
Up to now there are no established parameters for the follow-up of delayed radiation injuries1. Late toxicity is generally irreversible and can have devastating effects on quality of life of people exposed either accidentally or during therapeutic radiation treatments. They are the consequences of an imperfect tissue remodeling and of persistent radiation induced injuries2.
Histologically, late manifestations of radiation damage include fibrosis, necrosis, atrophy and vascular lesions. Although many etiologies have been suggested regarding these late toxicities, chronic inflammation has been described as playing a key role.
The recruitment of leukocytes from circulating blood is decisive in the inflammatory reaction. All the steps in the recruitment cascade are orchestrated by cell-adhesion molecules (CAMs) on both leukocytes and endothelial cells, and different subsets of CAMs are responsible for different steps in extravasation. The involvement of CAMs in many inflammatory diseases has led them to be considered as targets for therapeutic interventions3. However the long term alterations of CAMs expression in irradiated tissues remain unclear. Otherwise, a link between chronic low-level inflammatory responses and alterations in homeostasis of immunity are still demonstrable in the blood of A-bomb survivors. The most remarkable late effects of radiation were functional and quantitative abnormalities on T and B cells in survivors exposed to high doses4.
The following study was conducted to examine the response of the immune system in the inflammatory reactions of patients with late skin injuries after radiotherapy (Rt) or interventional fluoroscopy procedures.
The expression of adhesion molecules ICAM1 and β1-integrin on granulocytes and lymphocytes, as well as changes in subpopulations of T lymphocytes and the level of C-reactive protein, a well-studied inflammatory marker were evaluated.
METHODS
Patients From 1997 to 2011 over 160 patients were referred to the Radiopathology Committee of Hospital de Quemados del Gobierno de la Ciudad de Buenos Aires (Burn Hospital) for the diagnosis and therapy of Cutaneous Radiation Syndrome.The follow up of twenty one patients that showed late cutaneous reactions graded according to the RTOG / EORTC system is reported here.
Median age (ranges): 63 (49-79) years.
Late effect was considered from three month after the radiation procedure.
The study was approved by the Research and Ethics Committee of Burn Hospital. Informed consent was obtained from all patients.
Sample CollectionA total of 3ml of blood was collected into EDTA venous blood collection tubes (Vacutainer, BD) and maintained at room temperature until processed within 24h.
Flow CytometryThe expression of adhesion molecules ICAM1 and β1-integrin was measured by staining whole blood samples with a FITC-conjugated monoclonal antibody mouse anti-human ICAM1 (clone 15.2,Chemicon) and a FITC conjugated monoclonal antibody mouse anti-human INTEGRIN beta1 CD29 (clone TDM29, Chemicon), respectively.
The assessment of T(CD3+), T(CD4+) and T(CD8+) lymphocyte subsets was performed by staining with Tri-Test CD4-CD8-CD3 Reagent (BD) on whole blood sample.
After erythrocyte lysis with Facs Lysing Solution (BD) the samples were analyzed in a flow cytometer (BD FACS Calibur) using Cell Quest Pro Software.
CRP AssayThe level of CRP was measured on plasma samples with an immunoturbidimetric assay (Full Range CRP, RANDOX).
Statistical AnalysisNon-parametric analysis was carried out for groups' comparison by Kruskall-Wallis test. Comparison of two groups was done by Mann-Whitney U test. Significance was considered a
p value < 0.05.
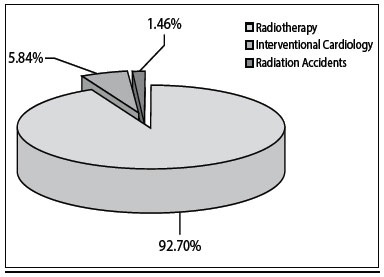
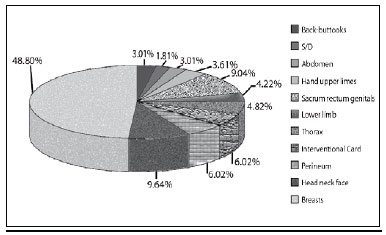
RESULTSThe distribution by etiology and location of the lesions are representative of all patients referred to the Burn Hospital during the period 1997-2011 (Figures 1 and 2).
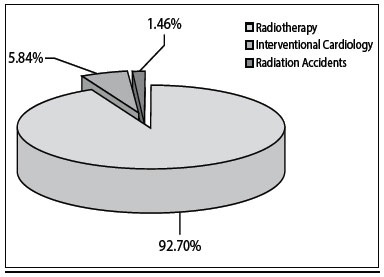
Figure 1 - Distribution by etiology of patients treated at Burns Hospital, period 1997-2011, N= 166.
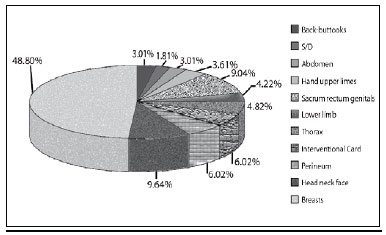
Figure 2 - Distribution by location of the lesion in patients treated at Burns Hospital, period 1997-2011, N= 166.
Late toxicity was evaluated according to the use of the RTOG/ EORTC Late Radiation Morbidity. Tissue: skin:
Grade 1: Skin slight atrophy; pigmentationchange; some hair loss;Grade 2: Patch atrophy; moderate telangiectasia; total hair loss;Grade 3: Marked atrophy; gross telangiectasia;Grade 4: Ulceration.
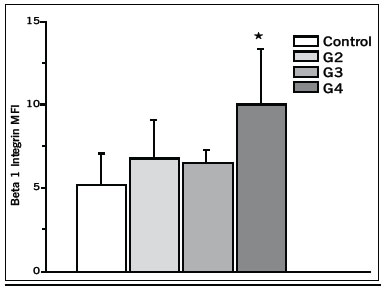
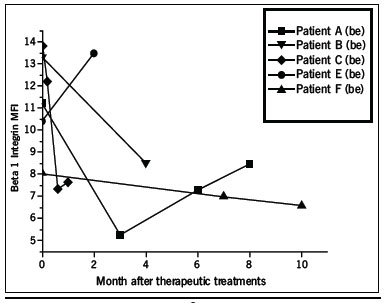
CAMs Analysis The analysis of adhesion molecules expression revealed a higher expression of β1 Integrin on gated lymphocytes of Grade IV patients compared to non-exposed controls (Figure 3). It was also noted a decrease in its expression value in the follow up of patients with good response to therapeutic treatment (Figure 4). There were no significant changes in the expression of ICAM1 neither lymphocytes nor granulocytes.
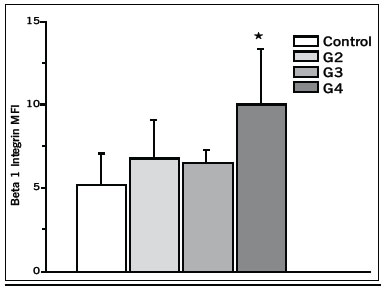
Figure 3 -β1 Integrin as Mean Fluorescence Index (MFI) on gated lymphocytes of patients graded according to RTOG/EORTC System (*p< 0.05 compared to control).
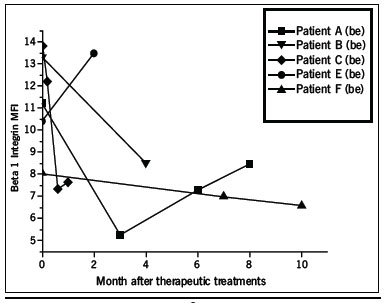
Figure 4 - Decrease in the expression of β1 Integrin in the follow up of patients with good response to therapeutic treatment.
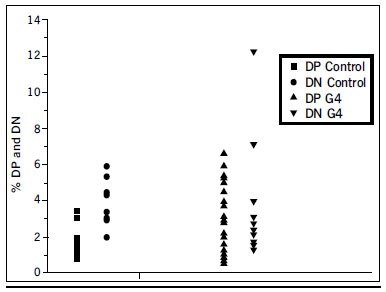
Three-color immunofluorescence flow cytometry of lymphocyte subsets did not show significant differences in the T(CD4+) / T(CD8+) ratio among the groups, including the control one. A distortion in the frequency of thymic precursors CD4-CD8- (Double negative DN) and CD4+CD8+ (Double positive DP) in peripheral blood was observed in G4 patients (Figure 5).
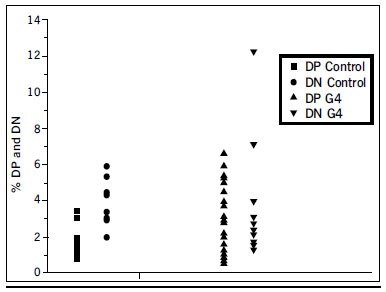
Figure 5 - Percentage of double positive and double negative thymic precursors in G4 patients and control sample.
Patient who underwent Rt for ovarian cancer during mid 1970s. Cyclical evolution with exacerbation crisis from 2000 up to now (Figure 6).
Figura 6 - Patient A.
Rt for thymoma in 1984. The patient presents at Burns Hospital in 2010 complaying from back pain and later ulceration since 2008 (Figure 7).

Figura 7 - Patient B.
Rt for angioma forty years ago. Ulcer recurrence over time (Figure 8).
Figura 8 - Patient C.
Radiation injury following interventional cardiology procedure reported as difficult, requiring prolonged duration of fluoroscopy (Figure 9).
Figura 9 - Patient D.
The level of C Reactive Protein (CRP), a widely used inflammatory marker, showed higher values in patients in acute phase (52.1±47.4mg/L*) and patients with late toxicity but in exacerbation crisis (13.5± 5.3mg/L*) with respect to patients with late radiation injury (1.9± 1.4mg/L) - (*
p < 0.01).
DISCUSSIONScientific evidences are supporting the view that leukocyte and endothelial cell-associated CAMs play a critical role in the vascular dysfunction and tissue injury associated with a wide variety of inflammatory diseases. The coordinated recruitment of leukocytes to sites of inflammation is largely governed by the time course and magnitude of CAMs expression.
The β1 Integrin is the major integrin expressed on resting T and B lymphocytes where as ICAM1 mediates both lymphocyte and monocyte adhesion but its expression is regulated on endothelial cells5.
We noted increased β1 Integrin expression on gated lymphocytes of patients that showed late cutaneous reactions graded 4 according to the RTOG / EORTC system and it had good correlation with the patient evolution. This findings differ from a previous study1 in two affected individuals, six years after a radiation accident, that revealed elevated levels of ICAM1 and β1 Integrin on gated granulocytes.
The main effectors of the adaptive cellular immune response are CD4+ and CD8+ T cells. We have not found significant changes in the ratio of the percentage of CD4+ and CD8+ T cells, although a tendency to a decrease was observed in the G4 group of patients compared to controls.
These cells derive from precursors migrating from the bone marrow to the thymus where single positive CD4 or CD8 naive T cells are selected in a maturation process. A small proportion of circulating CD4+CD8+(Double positive DP) or CD4-CD8- (Double negative DN) cells, representing immature T cells escaping from the thymus, has been described in humans6,7. Previous evidence has suggested that their frequency in blood can increase during several inflammatory disorders. The DP phenotype has been associated with high level of IL-4 production and enhanced extracellular matrix deposition by fibroblast8.
Our data show a tendency to higher values of both, DP and DN T cells on G4 graded patients compared with control donors. This suggests a disturbance in the T-Cell homeostasis although the role played in the radiation induced damage is still largely unknown.
CONCLUSIONSThe present findings show that the parameters analyzed, which require confirmation in a larger study, in combination with other inflammatory indicators could be used as potential follow-up markers of the chronic radio-induced inflammation process just as its response to therapeutic treatments.
REFERENCES 1. Scherthan H, Abend M, Müller K, Beinke C, Braselmann H, Zitzelsberger H, et al. Radiation-induced late effects in two affected individuals of the Lilo radiation accident. Radiat Res. 2007;167(5):615-23.
2. Gallet P, Phulpin B, Merlin JL, Leroux A, Bravetti P, Mecellem H, et al. Long-term alterations of cytokines and growth factors expression in irradiated tissues and relation with histological severity scoring. PLoS One. 2011;6(12):e29399.
3. Ulbricht H, Eriksson EE,Lindbom L. Leukocyte and endothelial cell adhesion molecules as targets for therapeutic interventions in inflammatory disease. Trends Pharmacol Sci. 2003;24(12):640-7.
4. UN. UNSCEAR 2006 Report.Volume II. Annex D. United Nations Publication. [Cited 2012 Dec 13]. Available from: URL: http://www.unscear.org/unscear/en/publications/2006_2.html
5. Krieglstein CF, Granger DN. Adhesion molecules and their role in vascular disease. Am J Hypertens. 2001;14(6 Pt 2):44S-54S.
6. Chen W, Ford MS, Young KJ, Zhang L. The role and mechanisms of double negative regulatory T cells in the suppression of immune responses. Cell MolImmunol.2004;1(5):328-35.
7. Nascimberti M, Pol S, Saunier B. Distinct CD4+ CD8+ double-positive T cells in the blood and liver of patients during chronic hepatitis B and C. PLoS One.2011;6(5):e20145.
8. Parel Y, Aurrand-Lions M, Scheja A, Dayer JM, Roosnek E, Chizzolini C. Presence of CD4+CD8+ double-positive T cells with very high interleukin-4 production potential in lesional skin of patients with systemic sclerosis. Arthritis Rheum.2007;56(10):3459-67.
1. Burns Hospital of Buenos Aires, Buenos Aires, Argentina.
2. Nuclear Regulatory Authority, Buenos Aires, Argentina.
Correspondence:
Mercedes Portas
Pedro Goyena 369 (1424)
Buenos Aires - Argentina
E-mail: mportas84@gmail.com
Article received: 10/10/2012
Article accepted: 5/1/2013
Work relesead at Hospital de Quemados del Gobierno de la Ciudad de Buenos Aires, Buenos Aires, Argentina.